Peripheral Venous Disease PVD Overview
Learn about Peripheral Artery Disease (PAD). Its causes, symptoms, treatments, and comparison with Peripheral Artery Disease (PAD) and Chronic Venous Insufficiency (CVI).
What is Peripheral Vascular Disease PVD?
Peripheral vascular disease (PVD) is a condition that affects blood vessels outside the heart and brain. Symptoms of vascular diseases that restrict blood flowing from an organ through arteries and veins. Doctors refer to it as peripheral vein disorders.
Patients who have PVD have a lower chance of relapse compared with those who don’t have a more severe disease. You may want to schedule an appointment with your physician to determine if your condition improves. Doctors diagnose or treat PVC (peripheral cardiovascular disease) with a symptom identification test.
How Does it Affect Blood Flow in the Legs?
PVD can cause parts of the body, like the brain, heart, arms, or legs leg muscles, to not get enough oxygen-rich blood through. Moreover, lower blood supply, causing symptoms such as pain, numbness, and skin changes.
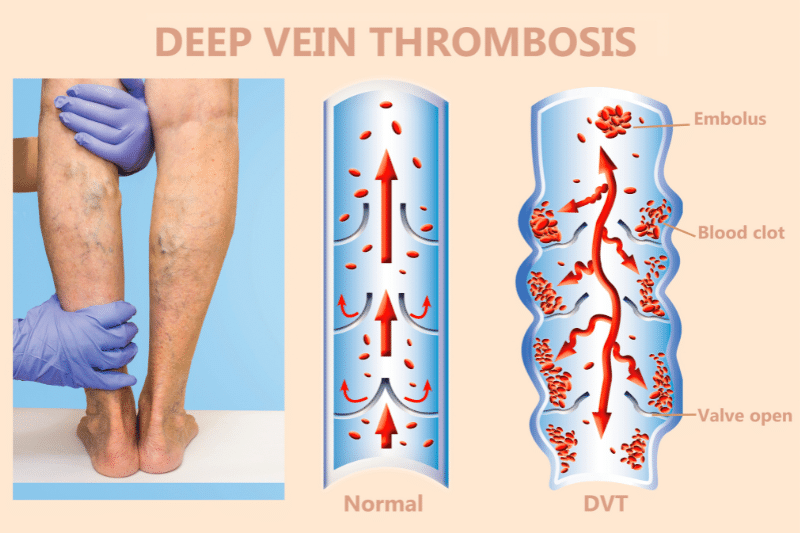
The legs and feet are most commonly affected, and other blood vessel or lymphatic vessels problems like deep vein thrombosis (DVT), varicose veins, and chronic venous insufficiency are linked to PVD.
What is PAD?
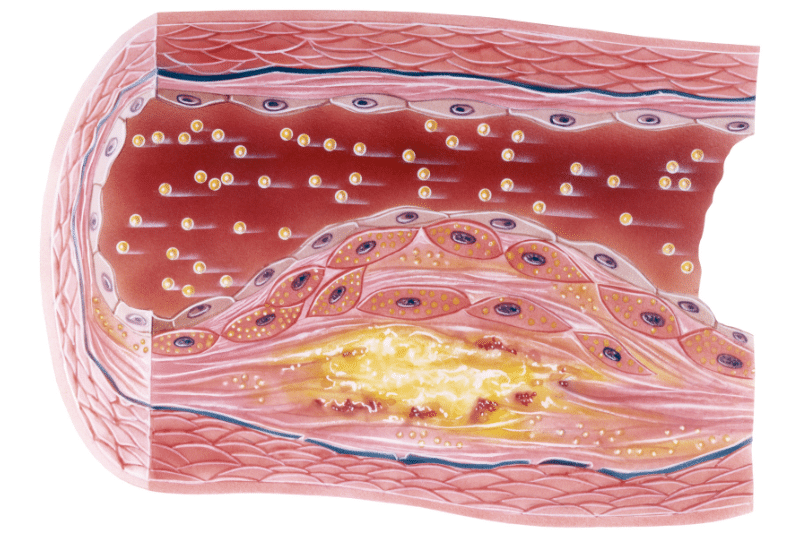
Peripheral artery disease (PAD) is a type of PVD that affects the arteries. Peripheral arterial disease is caused by plaques on arterial walls. If the plaque is thickened, the arteries will not increase blood flow or blood oxygen to the feet. PVD and PAD have been classified as a disease.
If excessive plaque builds up with time it blocks vascular walls or stifles blood flow in the body. PAD is not reversible. There’s minimally invasive therapy for PAD. When you are experiencing signs of pediatric ischemic disease, you should contact a vascular physician.
Peripheral Venous Disease (PVD) vs. Peripheral Artery Disease (PAD) – Key Differences
Several vascular diseases can cause a variety of complications from vascular damage to the peripheral vascular system, and those diseases can occur as a result of the loss of blood vessels. Although PAD is still, PVD is not always PAD.
The signs and risks for PVD are similar so understanding their differences and having them diagnosed is very important for everyone. While PAD specifically affects the arteries in the legs. Whereas PVD can affect blocked arteries in any blood vessel outside the heart and brain.
On the other hand, plaque buildup causes PAD, while PVD can have multiple causes. Such as atherosclerosis, blood clots, inflammation, infection, blocked or narrowed artery
Common Symptoms of PAD and PVD
Symptoms of PAD and PVD can vary depending on the severity of the disease and the location of the blockages in blood vessels. PAD and PVD can cause similar symptoms, including pain, numbness, and skin changes.
Peripheral Venous Disease (PVD) vs. Peripheral Artery Disease (PAD) – Key Similarities
There are several differences between PV and PAD in terms of the symptoms. People who have any of the conditions may feel leg pain, numbness, and cramping. They can diagnose and offer a personalized treatment plan with plans and programs that match your illness severity.
How to Identify Symptoms of Poor Circulation in the Legs?
Paying attention to specific symptoms can help tell the difference between PAD and PVD. However, chronic venous insufficiency (CVI) and deep vein thrombosis (DVT). These conditions or disorders can also cause symptoms.
Particularly, swelling and pain in the legs and ankles. It’s important to know the differences for a timely treatment at an early stage.
Common Risk Factors for PAD and PVD
Both PAD and PVD include risk factors. For instance smoking, high blood pressure, high cholesterol, and diabetes. A family history of PAD and PVD can also be a risk factor.
Chronic Venous Insufficiency (CVI)
CVI is a problem that affects the veins, a blocked artery or narrowed artery, that carries deoxygenated blood back to the heart. And doesn’t improve blood flow more freely back from leg veins to the heart. Instead of flowing backward, it tends to settle in the legs.
How Does CVI Relate to PAD and PVD?
CVI is a type of severe form of PVD that affects blood vessels in the veins. CVI can cause symptoms such as skin discoloration swelling and pain in the legs and ankles. Some patients with early-stage PAD or CVI have no problems or symptoms. However, the symptoms can vary. Focusing on specific symptoms can help distinguish PAD vs. CVA.
Peripheral Venous Disease (PVD) vs. Peripheral Artery Disease (PAD) – Diagnosis and Testing
Diagnosis for PAD and PVD typically involves a physical exam and medical history. Tests such as ankle-brachial index (ABI) and duplex ultrasound may also be ordered. Early diagnosis and treatment can help prevent serious complications and more severe heart disease.
Getting a diagnosis of ‘poor circulation’ in the legs. Depending on whether you have PADs or CVIs or in some cases coronary artery disease CAD. It is advisable to contact your doctor to discuss your medical and family history to assess your condition.
You may have to remove the socks or shoes so that if you have any concerns about your feet and legs you can get a blood pressure check. Diagnostics for PDA are similar. Your doctors will ask questions about your family history and your condition and perform a physical examination. It includes:
Tests for Peripheral Vascular Disease
Depending on the physician’s evaluation, the doctor may order a few tests to diagnose it. The ABI is based on a blood pressure test that looks at blood pressure in both the leg or arm to look at blood pressure in the legs and arms.
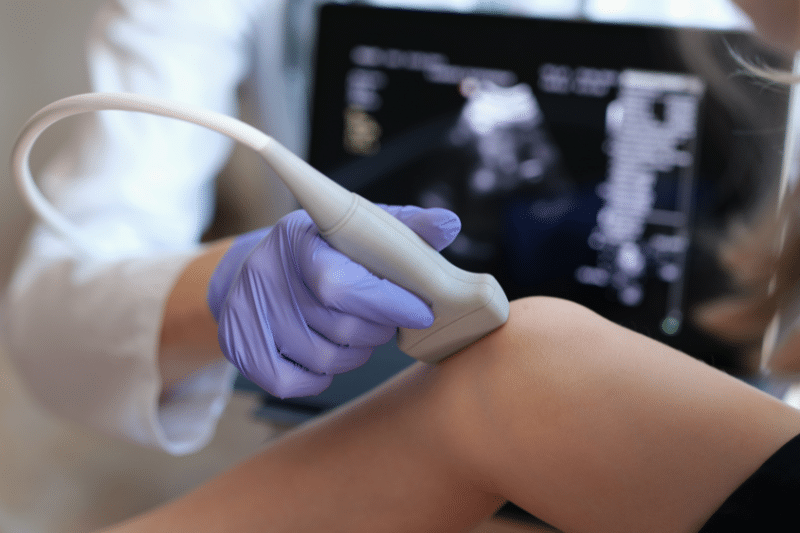
Ultrasound
The testing uses a sound wave that looks at blood flow and identifies obstructions of arteries and vein systems.
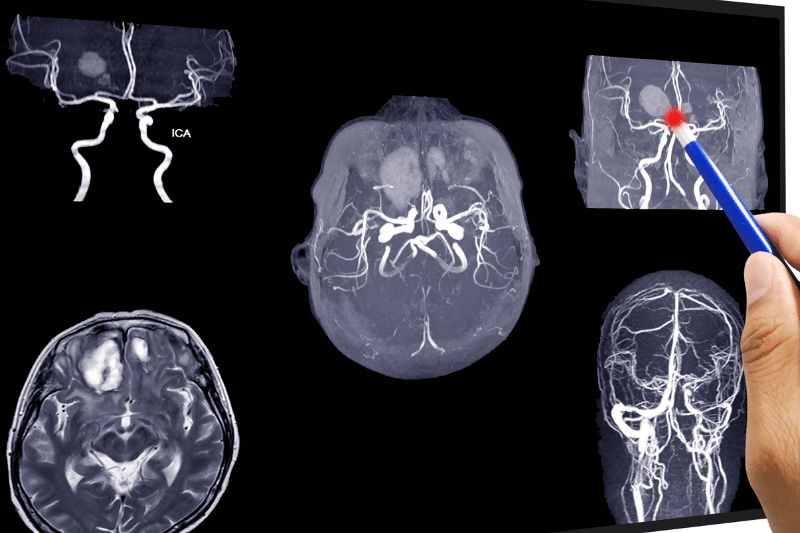
Magnetic Resonance Angiography
Medical providers inject contrast dyes in the arteries and take pictures for the detection of blockages. Moreover, it is possible to perform these tests using computer tomography or magnetron resonance.
A vascular surgeon may carry out another full bypass surgery, vascular surgery, or to re-establish vascular blockages with X-rays.
Tests for Chronic Venous Insufficiency
The doctor may be aware of CVI through an ultrasound of the heart attack leg arteries. To further determine how blood flows in these veins. However, sometimes it is needed more tests to find a cause if veins are not properly draining the blood flow to the heart.
Peripheral Venous Disease (PVD) vs. Peripheral Artery Disease (PAD) – Treatment Options
Treatment for PAD and PVD depends on the severity of the condition and the underlying cause. Individuals can maintain healthy blood flow and prevent a blood clot or other blood vessel or disease in their legs by following these guidelines:
-
Lifestyle changes, medication, and surgery are common treatment options.
-
Regular check-ups with a doctor can help identify risk factors and prevent PAD and PVD.
-
Maintaining a healthy diet and lifestyle to control high blood pressure. It can help manage symptoms and prevent complications.
-
Changing the diet and eating habits of people who have other diseases including diabetes, high cholesterol, and both high cholesterol and blood pressure.
-
Quitting smoking, regular exercise, maintaining a healthy weight, making healthier food choices, and keeping up with your treatment for other medical conditions.
Call us or schedule a teleconsultation. Nonetheless, our vascular physicians are trained to diagnose and treat PADs and PVDs at the IBI Dialysis and Vascular Access Center. Further preventing the higher risk of developing vascular-related complications or varicose veins condition. The medical team would also help you recommend minimally invasive procedures.










