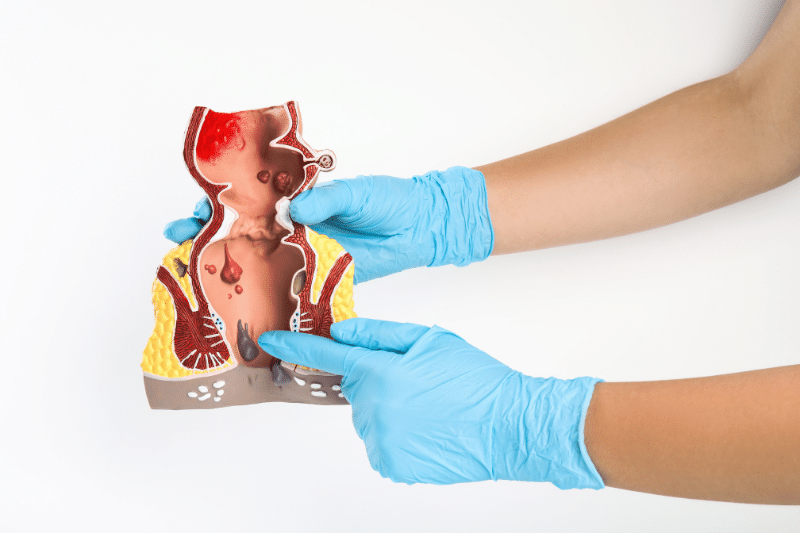
What is an Anal Fistula?
An empty anal canal or fistula is an abnormal tunnel under the front skin around part of the anus. Anal fistulas develop from anal gland infection, inflammatory bowel disease (such as Crohn’s disease), trauma, surgery, or radiation therapy near the anus.
That connects the anal canal in the colon to the skin of the anus, buttocks, and rectum. It is a small channel or connection. That forms between the skin near the anus and the external skin near the anus or the external opening of the anus and rectum.
What are simple fistulas?
Specifically, when it contains just the most muscle and has no branching. Colorectal surgeons refer to simple fistula surgery as fistulopathy. It’s a quick and easy solution to treating fistulated arteries (about 90%).
The fistula is cut from the rectum roof to allow the fistula to fill from underneath. It can even remove damaged skin. Cutting through an open roof can be painful, but it’s okay to cut through the muscle. Cutting excess weight may cause bowel problems.
Difference Between Anal Fistula and Anal Abscess
While an anal fistula often results from frequent infections from a previous or current. Some develop into abscesses and can become anal abscess or infection.
The anal canal plays a crucial role in the development of anal gland fistulas. Blocked or inflamed anal glands inside the anal canal or the skin around the anus can lead to an infection and abscess of anal glands. It can develop into an anal gland fistula. In some cases, surgeons also recommend examining issues underlying the digestive system or large intestine. To timely cure abscess.
Difference Between Anal Fistula and Anal Fissure
An anal fistula often causes persistent pain, swelling, and drainage of pus or blood from the opening near the anus. It can also cause fever and a general feeling of being unwell.
Whereas an anal fissure typically causes sharp pain during bowel movements, followed by a dull ache, and bleeding. Usually diagnosed by simply examining the tear in the anal lining. However, chronic fissures might require surgical procedures if they don’t heal with conservative treatments.
Rectal surgeons or colon surgeons diagnose both conditions through a physical examination. For an anal fistula, the colon and rectal surgeons may also perform MRI or an ultrasound to determine the extent of the fistula.
Causes of Anal Fistulas
Most anal fistulas are caused by an infection that starts in an infected tissue or an infected anal gland by itself. They can also develop as a complication of inflammatory bowel disease, such as Crohn’s disease. A fistula is a small tunnel that forms when pus is just under the skin along this drainage tract.
Risk Factors of Anal Fistulas
Crohn’s disease is a chronic condition that increases the risk of developing an anal fistula infection. The infection results in an abscess. Eventually, it drains on its own or the abscess is drained surgically through the skin next to the anus.
Who is at risk of developing anal fistulas?
Certain conditions require multiple surgeries or that affect the bowel control of other organs in the lower digestive tract or anal area. This may increase the risk of developing an anal fistula. These conditions require surgery including colitis, Crohn’s disease, and chronic diarrhea for colon and rectal cancer.
Surgical procedures for most anal fistulas should avoid dividing a large portion of the sphincter muscle to prevent problems with bowel control. If you develop an anal abscess. Then you have about a 50% chance of developing an anal fistula.
Symptoms and Signs of Anal Fistulas
Common or similar symptoms of most anal fistulas include:
-
Fever and chills.
-
Feeling tired and sick.
-
Pain and swelling around the anal area.
-
Redness, soreness, or itching of the skin around the anal opening.
-
Cyclical swelling, pain, and drainage of pus or blood from the wound area.
Moreover, fecal incontinence is most likely if surgery removes some of the muscle around the anal opening. Proper treatment and follow-up care can manage complications.

Diagnosis and Treatment of Anal Fistulas
A healthcare provider may refer you to a specialist who specializes in colon and rectal diseases. The specialist will ask about common symptoms and medical history.
Treatments for anal fistulas depend on their involvement with the sphincter muscles, which helps determine the appropriate surgical procedure.
How do surgeons perform the procedure?
The surgeon will perform a physical exam and look for a fistula opening near the anal opening. Consequently, they will also use imaging tests and studies to help with the diagnosis, such as a fistula probe, anoscope, or imaging studies like ultrasound or MRI in the operating room. It can be drained surgically.
Surgical and Non-Surgical Treatment Options
Individuals with Crohn’s disease, usually developed anal fistulas. Surgical treatment options include fistulotomy. Particularly, filling the fistula near the anus with a special glue or plug, reconstructive surgery, seton placement, and medical therapy.
However, treatment options depend on the size and location of the fistula, as well as the individual’s overall health.

Managing Fistula Symptoms
Lifestyle changes to manage symptoms include:
1. Finish all of your antibiotics.
2. Take pain medicine as directed by your surgeon.
3. Don’t take any over-the-counter medicines without first talking to your provider.
Other important instructions may include soaking in a warm bath and wearing a pad over the anal area. Additionally, eating a diet high in fiber and drinking plenty of fluids can also help. Besides this, use a stool softener or bulk laxative as needed.
Importance of Follow-up Care After Procedure
Follow-up care is crucial to ensure that the anal fistula is healing properly and to prevent complications.

Complications and Prevention
If individuals cannot control bowel movements. Then they are likely to have fistula recurrence. Moreover, it is most likely that surgery removes some of the muscle around the anal opening. Proper treatment and follow-up care can manage complications.
How to prevent anal fistulas from recurring?
-
A healthy diet and regular exercise.
-
Prevention includes maintaining good hygiene and avoiding constipation.
-
Avoiding trauma to the anus and surrounding area can also help prevent anal fistulas.
When to Seek Medical Attention
If you experiencing signs that indicate the need for urgent medical attention. Then call your healthcare provider if you have symptoms of an anal fistula. Especially if you have a history of previous anal abscesses.
Subsequently, if you have been treated for an abscess or fistula. Then let your colorectal surgeon know right away. However, early treatment is crucial to prevent complications of liver disease. As well as promote proper healing.

Post-Treatment Prognosis
Despite proper treatment and complete healing, an abscess or a fistula can come back. However, if an abscess comes back, it suggests that perhaps there is a fistula that needs to heal completely.
If a fistula comes back, then additional surgery will likely be required to treat the problem. Diagnosis and treatment by colon and rectal surgeons are crucial to prevent complications and promote proper healing.
Call us or schedule a teleconsultation to learn more about minimally invasive fistula laser treatment.










