This guide is to help with surgical stomach operations related to bariatric surgery. Helping individuals make informed life-changing decisions about metabolic and bariatric surgery procedures.
What is stomach surgery or stomach operation?
Stomach surgery, also known as metabolic and bariatric surgery. These surgeries or weight loss procedures help to lose weight. alter the stomach’s connection from blood sugar to the digestive system to limit food intake or nutrient absorption.
Furthermore, helps you reach and maintain a healthy weight. Each surgical procedure is different and suitable for different patients.
What is stomach removal called?
Bariatric surgeon remove part of the whole stomach and refer to it as a gastrectomy. Depending on the size and extent of the abdominal surgery done. The surgeon performs gastrectomies or Bariatric procedures under local or general anesthesia. To treat stomach cancer, severe ulcers, or other serious stomach conditions.
Surgical Stomach – Bariatric Surgery Reasons and Need for Surgery
Why Would a Person Need Stomach Surgery?
A person may need stomach surgery for many reasons, mainly when other treatments don’t work. Severe obesity is a big one, bariatric surgery is a solution for significant and sustainable, weight loss surgery.
Stomach cancer which the American Cancer Society states affects around 27,600 Americans every year. Often requires a surgery to remove the malignant tissues and prevent the cancer from spreading.
Individuals with severe and chronic stomach ulcers who don’t respond to medication or lifestyle changes may also need surgery. These ulcers can cause bleeding, perforation, or obstruction. This may require surgical repair or removal of the affected part of the stomach.
Can Stomach Ulcers Require Surgery?
Yes, stomach ulcers can require surgery. Especially when they become severe and complications arise. Chronic peptic ulcers that don’t heal with medication. Furthermore causes bleeding, perforation, or blockage of the digestive tract.
These complications need surgical intervention to repair the damage or remove the ulcerated part of the stomach. For example, according to the American Gastroenterological Association. About 10% of peptic ulcers may require surgical treatment due to complications.
The major surgery itself may involve procedures like vagotomy, pyloroplasty, or partial gastrectomy. To remove the ulcer and reduce acid production in the stomach.
Surgical Stomach – Bariatric Surgery Medical Conditions Treatment
What Stomach Problems Require Surgery?
Stomach surgery addresses severe obesity and obesity-related conditions. Especially when lifestyle changes and medications don’t produce significant results.
Other conditions include heart disease, stomach cancer, severe peptic ulcers, and gastrointestinal disorders like Crohn’s disease. For example morbid obesity, according to the Centers for Disease Control and Prevention (CDC).
Nearly 40% of adults in the US are individuals with heavier body weight. That’s how big the need for weight loss surgery is for effective treatments including weight loss surgery alone.
What Can Be Treated with Stomach Surgery?
Healthcare providers treat several medical conditions with stomach surgery:
-
Chronic Peptic Ulcers – When ulcers don’t respond to other treatments. Then the surgery can repair or remove the ulcerated part of the stomach.
-
Gastric Obstruction – Surgery can remove blockages in the stomach or intestines caused by tumors, scar tissue, or other abnormalities.
-
Stomach Cancer – Surgical removal of cancerous tissue from the stomach often necessary. To stop the spread and improve survival rates. This may be partial or total gastrectomy.
-
Severe Obesity – Bariatric surgery helps with weight loss and has fewer risks related to obesity. Gastric bypass, sleeve gastrectomy (gastric sleeve surgery), and adjustable gastric band surgery are common.
-
Gastrointestinal Disorders – Conditions like Crohn’s disease and severe cases of acid reflux, gastroesophageal reflux disease (GERD). Mainly causes complications that may require surgery.
Surgical Stomach – Bariatric Surgery Types
Gastric Bypass (Roux-en-Y)
Gastric bypass involves creating a small stomach pouch called metabolic and rerouting a part of the small intestine to this small pouch itself. Evidently, it reduces the size of the stomach and the length of the digestive tract that food passes through. As a result, reduces calorie absorption.
Benefits and Risks
Gastric bypass can result in significant weight loss and improvement of obesity-related conditions like type 2 diabetes. But it has risks like nutrient deficiencies and dumping syndrome. Particularly, where food moves too quickly from the stomach to the intestines.
Success Rate
A study by the National Institutes of Health (NIH) found that patients who had gastric bypass. Eventually lost an average of 60-80% of their extra weight loss in 2 years. Besides this, many also saw improvement in their high blood pressure and cholesterol levels.
Sleeve Gastrectomy
Sleeve gastrectomy (vertical sleeve gastrectomy) removes about 80% of the stomach, leaving a tube or stomach pouch. This reduces the remaining stomach part’s capacity and the hormones that control hunger and fullness.
Benefits and Risks
This procedure results in a lot of weight loss and fewer nutrient absorption complications than a gastric bypass surgery. But it’s irreversible and has risks of staple line leakage and nutritional deficiencies.
Hormonal Impact on Hunger
A JAMA Surgery study shows that sleeve gastrectomy reduces ghrelin, the hunger hormone. Therefore, patients feel less hungry and eat healthy foods with fewer calories.
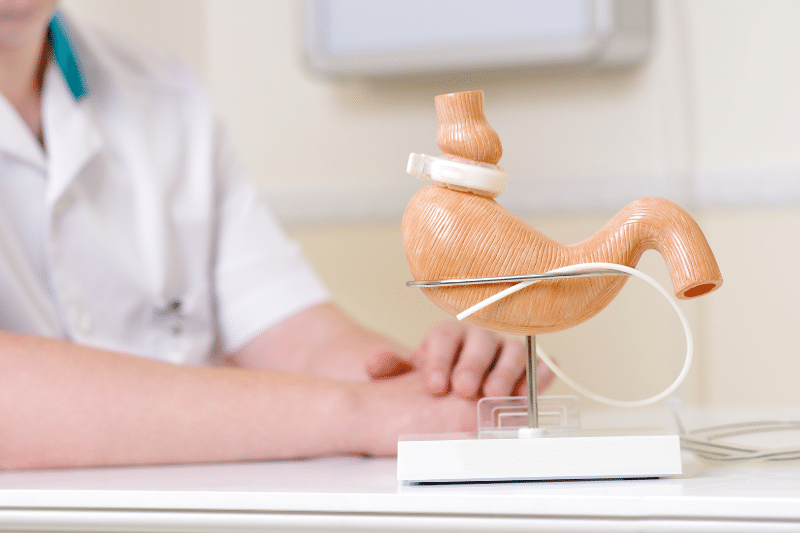
Adjustable Gastric Banding
Adjustable gastric banding involves placing a gastric band all around the top of the stomach to create a small pouch. Later the adjustable gastric band itself adjusts. To further the gastric band can control the flow of food so patients feel full sooner and eat less.
Benefits and Risks
Less invasive and reversible. Shorter recovery time but may result in less rapid weight loss, than other bariatric surgeries. Band slippage, erosion, and infection.
Patient Outcomes
According to the American Society for Metabolic and Bariatric Surgery (ASMBS). Patients with gastric bands lose about 40-50% of their excess weight. Although, the procedure has declined in popularity. As sleeve gastrectomy has become more popular.
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
biliopancreatic diversion with duodenal is a more extensive surgery. The second surgery combines a sleeve gastrectomy with a re-routing of the intestines to limit food absorption. Additionally, this robotic surgery reduces the size enough weight of the stomach and changes the digestive process.
Benefits and Risks
In fact, diversion with a duodenal switch has the highest weight loss and improvement in obesity-related conditions. But has a higher risk of complications and nutritional deficiencies. Subsequently, patients will need lifelong vitamin and mineral supplements.
Long-term Success
A study in the Obesity Surgery journal found that patients who had BPD/DS. They had an average excess weight loss of 70% after 5 years. Consequently have a significant improvement in diabetes and hypertension.

Surgical Stomach – Pre Bariatric Surgery Eligibility and Requirements
-
Medical Checkup – Full medical assessment. Blood tests, imaging, and specialist consultations if required.
-
Psychological Evaluation – Candidates undergo a psychological evaluation to ensure they can adapt to the big lifestyle changes after surgery. Mental health support is key to long-term success.
-
BMI and Health Conditions – Candidates for bariatric surgery have a body mass index of 40 or higher. Even a BMI of 35 or higher with obesity-related conditions. For instance type 2 diabetes, hypertension, or sleep apnea.
-
Physical Activity – Increasing your physical activity before surgery will help with your surgical outcome. Further, it establishes the habits for long-term weight management.
-
Smoking Cessation – Smoking increases the risk of complications and impairs healing. You must quit smoking before surgery.
-
Nutritional Counseling – You will meet with a dietitian to learn about the dietary changes. Then you will need to make a plan for before and after surgery. This includes a high protein, low sugar diet and eating smaller, more frequent meals.
Surgical Stomach – Post Bariatric Surgery Considerations
Life and Adaptation
-
Immediate Post-Surgery Diet – Patients start with a liquid diet, then pureed foods, and soft foods. Eventually solid foods over several weeks. This phased approach promotes the body’s ability to adjust to the smaller stomach.
-
Long-term Dietary Guidelines – A long-term diet is high in protein and low-carbon carbohydrates. Patients must avoid high-sugar and high-fat foods to prevent dumping syndrome and other complications.
-
Tailored Exercise Programs – Bariatric surgeons customized exercise program to further speed up the recovery process. Additionally, helps patients to build strength and endurance while avoiding injury. Lastly encouraged to do daily low-impact aerobics and exercises.
Aftercare and Follow-Up
-
Regular Medical Check-Ups – To make sure you’re doing well and catch any issues early.
-
Nutritional Monitoring – Blood tests and dietitian consultations to monitor nutritional status and adjust supplements as needed to prevent deficiencies.
-
Counseling and Support Groups – This helps you navigate the emotional ups and downs of life after surgery. Talking to others who have been through the same thing is so helpful.
-
Monitoring and Adjustments – Continuous mental health monitoring is key. Healthcare providers will adjust support as needed to address depression, anxiety, or eating disorders.
Long-Term Outcomes and Considerations
-
Losing Weight – Most bariatric surgery patients able to lose weight in the long term. According to the ASMBS, patients typically retain 50-60% of excess weight loss 5 years post-surgery.
-
Comorbidities – Bariatric surgery often results in significant improvement in obesity-related conditions. Many patients go into remission of type 2 diabetes, lower blood pressure, and improved cardiovascular health.
-
Better Daily Living – Patients often report an overall better quality of life after surgery. More mobility, more energy, and higher self-esteem contribute to overall well-being.
-
Nutritional Deficiencies – Long-term risks include nutritional deficiencies that will require lifelong supplementation. Monitoring helps to minimize these risks.
-
Surgical Risks – While complications are rare they can include infections, hernias, or gastrointestinal issues. Get medical attention quickly if you have any.

Surgical Stomach – Bariatric Surgery Recovery
How long is the Recovery Time for Stomach Surgery?
Recovery time after stomach surgery depends on the surgery and how much weight your health is. Minimally invasive surgeries like lap band or sleeve gastrectomy have shorter recovery times than open surgery.
You can expect to be back to normal in 3-6 weeks after surgery. But full recovery including adjusting to new eating habits and lifestyle changes takes several months. Recovery time factors include:
-
Patient’s Health – Pre-existing conditions can slow down recovery.
-
Post-operative Care – Following post-op guidelines affects recovery time.
-
Type of Surgery – Laparoscopic has a quicker recovery time than open surgery.
Surgical Stomach – Bariatric Surgery Hospital Stay
How Long do you stay in the Hospital for Stomach Surgery?
Hospital stay in a recovery room after stomach surgery also varies by surgery. For laparoscopic surgery, the hospital stay is 1-3 days. Open surgery is 5-7 days. We want to monitor you for any immediate post-op complications.
In addition, make sure you can manage pain and start dietary changes before discharge. However, discharging criteria include medical condition:
-
Mobility – Can walk and do basic self-care.
-
Pain Management – Can manage pain with oral meds.
-
Stable Vitals – Blood pressure, heart rate, and temperature normal.
-
Diet Tolerance – Can tolerate liquids and soft foods without nausea or vomiting.

Surgical Stomach – Bariatric Surgery Post Operative Care
What are the Post-Operative Care Tips After Stomach Surgery?
Post-op care is key to a smooth recovery. Here are the tips:
Diet and Nutrition
-
Small Meals – Eat small portions to avoid discomfort and aid digestion.
-
Gradual Diet Progression – Clear liquids, then pureed foods, then soft solids.
-
Hydration – Drink plenty of fluids but don’t drink with meals to avoid overfilling the stomach.
Physical Activity
-
No Heavy Lifting – No heavy lifting for 6 weeks post-op.
-
Early Ambulation – Walk as soon as possible to prevent blood clots and promote healing.
Wound Care
-
Keep incisions clean and dry – Follow dressing changes and watch for signs of infection.
-
Monitor for complications – Watch for fever, swelling, or drainage from the incision site.
How much pain is the recovery from Stomach Surgery?
Pain varies with both the size and type of laparoscopic surgery and individual pain threshold. Most patients will have some discomfort and pain for the first few days post-op. Although, laparoscopic surgeries have less pain than open surgeries due to smaller incisions.

Surgical Stomach – Bariatric Surgery Post Operative Complications
What are the Common Complications During Recovery from Stomach Surgery?
Infection
Infections at the incision site or within the abdomen are possible. Symptoms include redness, swelling, pain, and fever. Keeping the surgical site clean and following wound care instructions can help prevent infections.
Blood Clots
Post-surgery immobility increases the risk of blood clots. Early ambulation, leg exercises, and possibly blood-thinning medications are preventive measures.
Nutritional Deficiencies
Since bariatric surgeries affect nutrient absorption, patients might develop deficiencies in vitamins and minerals. Such as B12, iron, calcium, and vitamin D. However, regular monitoring and supplementation are essential.
Dumping Syndrome
Especially common after gastric bypass surgery, dumping syndrome occurs. When food moves too quickly from the stomach to the small intestine. Moreover causing nausea, diarrhea, and dizziness. Nonetheless, eating small, frequent meals can help manage this condition.
Anastomotic Leaks
In surgeries like gastric bypass, leaks at the surgical connections to the small intestine can occur, leading to severe infections. Symptoms include abdominal pain, fever, and rapid heart rate. Then doctor’s practices recommend immediate medical attention.
Considering bariatric surgery, call us or schedule a teleconsultation. Our board-certified bariatric surgeons use minimally invasive surgical techniques. They will guide you on what to do based on your health conditions, lifestyle habits, and goals.










